by Isabella Benn
Are you interested in learning about lasting mental health challenges as COVID-19 cases decline? If you’re like most people who have likely struggled with mental health during this pandemic, continue reading. Mental health care can be complex and confusing to access. However, connecting with a team of professionals that specialize in navigating behavioral health makes the process significantly less stressful.
In this blog, we’ll discuss the long-term impacts of COVID-19 and how it affects your mental health. Before we dive in, make sure to subscribe to our quarterly newsletter to stay up-to-date with current news, articles, policy changes, and helpful information.
Now, let’s discuss mental health issues amid lower COVID-19 cases.
Most people are experiencing the negative impacts associated with the pandemic and economic difficulties. Individuals already struggling with substance use and mental health disorders pre-pandemic are now facing additional barriers to care. Before the pandemic, one out of ten individuals in the United States showed signs of depression or anxiety. During the pandemic, approximately four out of every ten adults in the U.S. reports symptoms consistent with depression and anxiety disorders. A 2020 poll administered by the Kaiser Family Foundation showed that individuals experienced increased challenges with poor sleep, unhealthy eating habits, increased substance use, and exacerbated chronic health conditions.
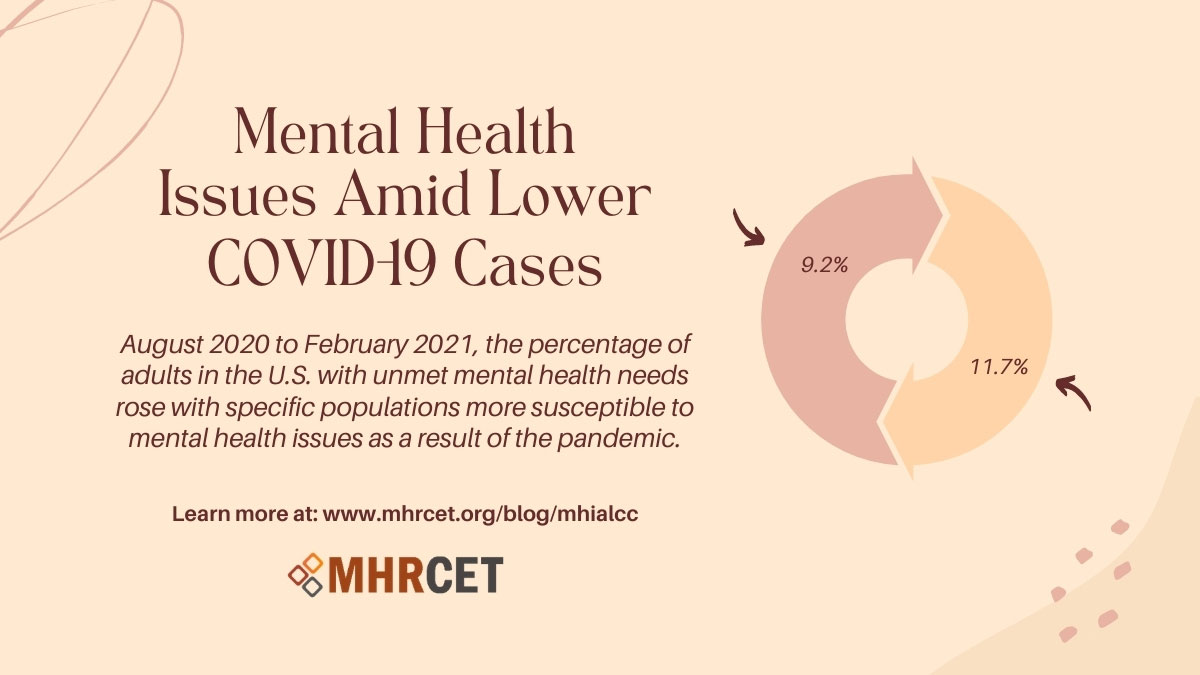
From August 2020 to February 2021, the percentage of adults in the U.S. with unmet mental health needs rose from 9.2% to 11.7% with specific populations more susceptible to mental health issues as a result of the COVID-19 pandemic. Adults that did not graduate high school and young adults ages 18-29 documented increased mental health symptoms and barriers to care.
People are working through death anxiety, social anxiety, loss of loved ones, feelings of being unsafe, and a complete disruption of society as we knew it. Dr. Ksera Dyette warns that people should be mindful of what she calls “the crash.” During a traumatic event emotional processing is on hold. Once the sense of danger dissipates a crash occurs when the mind and body can begin feeling and processing.
COVID-19 trauma has temporarily masked mental and physical health conditions. PTSD, nightmares, and flashbacks are critical concerns for first responders. Everyone should be mindful of the adjustment period in terms of social contacts and energy levels.
The collective global trauma everyone is experiencing must be considered at all points of care, including crisis response, hospitalization, and outpatient mental health treatment. All things considered, once the virus is gone the trauma and mental health issues will remain.
References
https://www.cdc.gov/mmwr/volumes/70/wr/mm7013e2.htm?s_cid=mm7013e2_w